It’s getting harder for patients to find a doctor as wait times and barriers to access grow
By Meera Madadevan, Granite State News Collaborative
About three years ago, Loren Selig, a Durham resident and mother of two college-aged daughters, went from having one family physician for her, her husband and their kids since the time their children were born to receiving medical care from nurse practitioners. The change happened after their doctor’s practice was purchased.
Kylee Rock, 23, moved to Dover from Tilton a few years ago. She is so afraid of not being able to find a local primary care doctor – given negative stories she has heard -- that she still drives an hour to see her doctor in Concord, even though she works full-time and finds it hard to do so.
Rachel Legard, a 63-year-old Lee resident, routinely jots down names of highly recommended primary care doctors whenever she hears about one from friends because, as her own doctor nears retirement age, she too is afraid she’ll be stuck without a doctor soon.
All three are trying to adjust to an acute shortage of primary care doctors that lingers on in New Hampshire and nationally. Some say it is reaching a crisis point.
“We used a family practitioner from when our kids were babies rather than a separate pediatrician,” said Selig. “We had one doctor for all of us, and it was a model we really liked, but our doctor’s practice got swallowed up by [Beth Israeli Lahey-owned] Core Physicians, and the level of personal care we noticed changed at that point, from having one where they would take their time with us to a ‘You’ve got 15 minutes’ kind of thing. … It’s been challenging on all sorts of levels.”
Interviews with about a dozen patients reveal nervousness and frustration over not being able to find a doctor who not only is accepting new patients but also over experiencing long wait times to get an appointment. Some patients likened the primary care doctor to the role of the wizard from “The Wizard of Oz.” “You know he’s there, but you never see him,” said Holly Breton of Rochester.
Access is just part of the problem. Primary care doctors themselves are under enormous pressure to see more patients in a shorter time, face mounting administrative burdens, and are paid far less in reimbursements than their specialist counterparts.
“Things were a lot simpler back then,” said Dr. Sangita Agarwal, a family physician who works in Seabrook and has been a family doctor for 30 years. “It was easy to submit to insurance companies because there were only a handful of insurers back then. We felt we could concentrate more on our practice and our patients. … Now, we are practicing medicine with prior authorizations, which have taken on a life of their own.”
A crucial lifeline for patients
A shortage of primary care doctors – amid an overall physician shortage – has been brewing for several years. What is new is that the shortage is being exacerbated as health care consolidation intensifies in New Hampshire and corporate ownership of physician practices rises.
In fact, to adequately meet health care needs, New Hampshire will need an additional 333 primary care physicians by 2030 – a 29% increase from 2010, when there were 110 so-called PCPs, according to data from the Robert Graham Center for Policy Studies, a primary care research arm of the American Academy of Family Physicians. New Hampshire’s PCP ratio is one doctor per 1,247 people, which is lower than the national average of one doctor per 1,463 people, according to the same report.
But compared to the rest of New England, New Hampshire appears to have the greatest need. The Graham Center report projects that Vermont needs an additional 119 primary care physicians by 2030, a 19% increase from 2010. Maine needs an additional 120 PCPs, a 9% increase. Massachusetts needs 725 PCPs, a 12% increase. Rhode Island needs 99 PCPs, an 11% increase. And Connecticut needs 404 PCPs, a 15% increase.
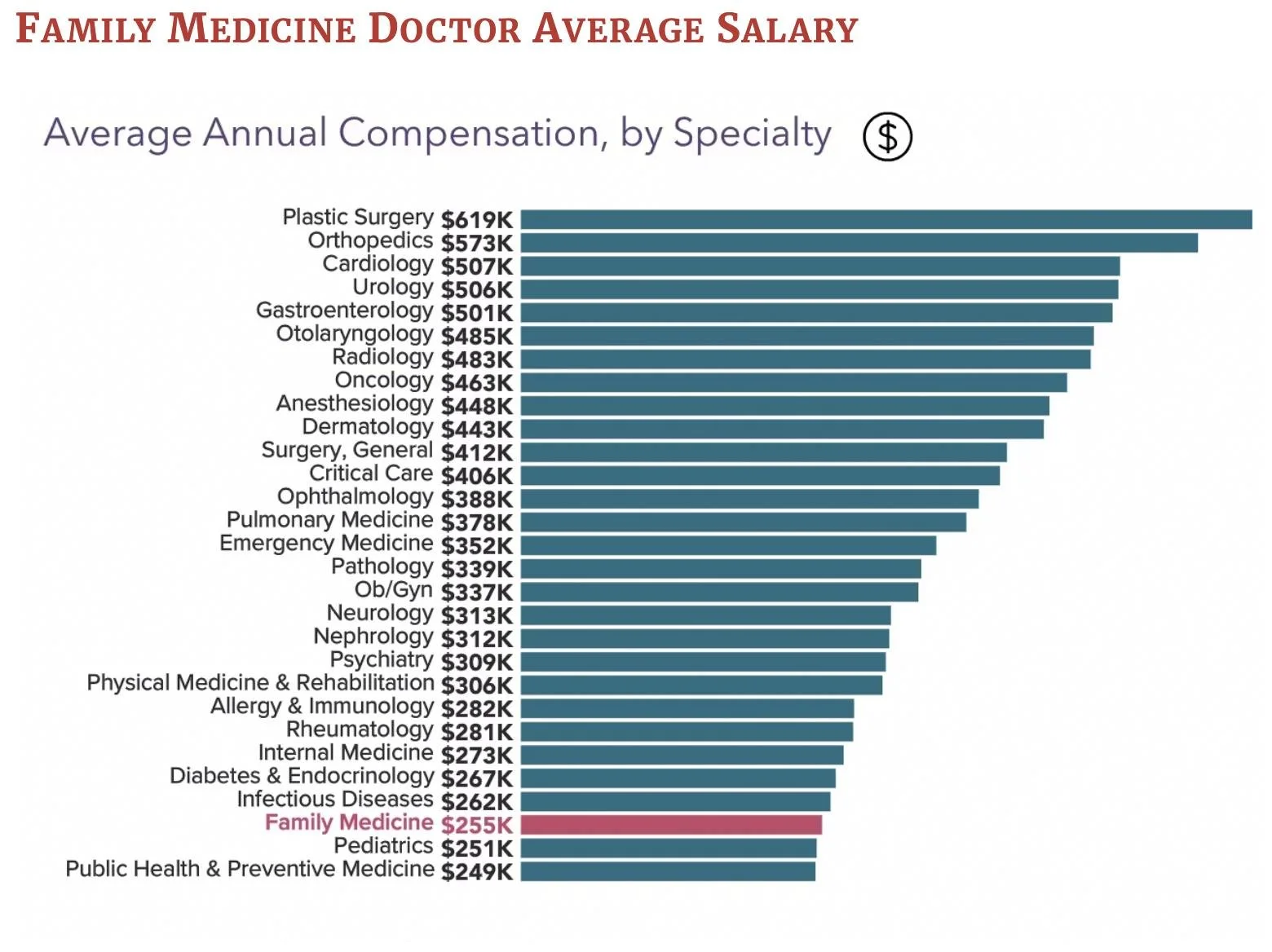
Shown are annual average salaries by medical specialty for physicians in the U.S. (White Coat Investor)
While the N.H. Department of Health and Human Services acknowledges the shortage of primary care doctors, it says that the state ranks fifth in the nation when it comes to the number of primary care providers per 100,000 people, citing a study by United Health Foundation, an arm of United Health Group, the nation’s largest health insurer. That number includes doctors and other primary care providers, such as nurse practitioners and physician assistants.
Citing 2022 numbers, the 2024 Annual Report on the NH Health Care Workforce and Data Collection said the number of physicians in the state grew by a modest 5.5%, while the number of nurse practitioners grew by 42% and physician assistants grew by 16.6%.
Primary care physicians – defined broadly as family physicians, pediatricians, geriatricians and general practitioners – play an integral role in not only diagnosing and helping to manage illnesses like heart disease, hypertension, diabetes and asthma, but also provide preventive care with routine checkups, risk assessments, screening tests and helping patients maintain an overall healthy lifestyle. They are also often a patient’s link to getting referrals and coordinating care with specialist doctors, who also often have long wait periods for appointments.
“The fact of the matter is that when there’s a primary care doctor in a ZIP code, the life expectancy of the people in that ZIP code increases,” said Dr. Maria Ramas, a family physician and a medical consultant. She is also a member of the state’s Healthcare Consumer Protection Advisory Commission that was recently created to assess the impact of hospital consolidations in New Hampshire.
Despite their vital role, primary care physicians are among the lowest paid doctors in the industry.
“I think there’s a movement to try and figure out how to better compensate for primary care, because we really undervalue and under-invest in primary care,” said Lucy Hodder, director of the Health and Life Sciences Law and Policy programs at the University of New Hampshire’s law school. “We just pay them peanuts compared to what we pay specialists because of the way we reimburse physician services with RVUs.”
RVU, or relative value unit, is a system used to measure and value the time, effort, complexity of a procedure and expertise required to provide a specific medical service. Government programs such as Medicare and private insurers use RVUs to determine physician reimbursement. They can also be used to track physician productivity and efficiency.
Adding to the complexity of the physician shortage is New Hampshire’s health care landscape, which is changing dramatically, due to mergers and acquisitions sweeping the industry as larger hospital systems, insurers and private equity firms buy up physician practices.
“If there is a change in ownership, there may be a change in mission and a change in support to reimburse and compensate and invest in primary care, mental health, substance abuse, eldercare, etc,” Hodder said. “You may see practices that are hospital-owned focusing on higher-end surgeries, cardiac services, inpatient ICU care, oncology, orthopedics. None of that is primary care, so I think that’s why when there’s a hospital merger, there’s a real question about to what extent is there a commitment to invest in primary care.”
In 2024, the percentage of doctors nationwide who were in private practice dropped to 42.1% from 60.1% in 2012, according to the American Medical Association’s most recent Physician Practice Benchmark Physician Practice Benchmark Survey This means that around 80,000 fewer doctors were in private practice in 2024 than in 2012, growth of the physician population notwithstanding, the association said.
The share of doctors employed at hospital-owned practices increased to 34.5% in 2024 from 23.4% in 2012. Doctors in the survey cited a need to better negotiate higher payment rates with insurance companies and to lessen costly resources as the top two reasons for no longer owning their own practices.
Possible solutions
Experts cite several reasons for the increased demand for and shortage of primary care doctors. Topping the list is New Hampshire’s aging population. It is aging faster than nearly every other state, and that shift is already influencing not only health care but also housing issues, according to the NH Fiscal Policy Institute.
As the general population ages, so are primary care doctors themselves. Many are nearing retirement age, and there is concern that there are not enough medical students and residents in the pipeline to replace them.
There has also been an increase in the number of people with health insurance, due to the Affordable Care Act, and that increases demand. But that could change with current federal budget cuts.
And, because it’s not financially lucrative, fewer medical students and residents are opting for primary care, reducing the pool of doctors in the pipeline.
What are policymakers doing to help alleviate the state’s primary care workforce shortage?
In 2010, legislators established an ongoing commission called the Interdisciplinary Primary Care Workforce to help assess and recommend policies and programs to strengthen the number of providers serving the state’s rural areas. The 20-member commission continues to meet monthly.
According to a 2021 Primary Care Needs Assessment report published by the state Department of Health and Human Services, the state is prioritizing efforts to create a clinical placement program, a rural residency track and getting additional funding for the State Loan Repayment Program. It is not clear whether the state has made any progress with these initiatives.
The State Loan Repayment Program, which secured $300,000 in 2024, provides funds to health care professionals working in areas of the state designated as medically under-served and who are willing to commit to working a minimum of three years there. However, funding for the program is at the mercy of lawmakers and annual state budget approvals.
The state also created a Health Professions Data Center to collect data on how many primary care providers actually work in the state and where they do that work.
In a 2024 report, the Division of Public Health pointed to data collected by the Health Professions Data Center and said it pointed to “an anticipated decline in the primary care physician workforce, especially in rural communities.”
It added: “Despite these physician workforce challenges, the APRN (nurse practitioners) and PA (physician assistant) workforce demonstrate continued growth and primary care reinforcement.”
That logic, however, falls on deaf ears, for patients who want the expertise and training of a medical doctor.
“I’m not saying nurse practitioners don’t know what they’re doing, but it does seem there’s a level of training I’m not getting if I see a nurse practitioner, said Ruth Sample of a Lee, an associate professor of philosophy at UNH whose family had the same family practitioner for about 15 years and has been switched to a nurse practitioner.” So far it’s been OK because I’m not a sick person, but I don’t have the same level of confidence.”
She added: “I don’t know what this all means. If doctors retire, is this just how primary care is going to be?”
This story is part of Critical Condition: What hospital consolidation means for care, access, and your community, a special series co-produced by partners in the Granite State News Collaborative. These stories are being shared by media outlets across New Hampshire. We want to hear from you! Take our short survey at https://tinyurl.com/3au39uct about your healthcare experiences. For more information, visit collaborativenh.org.